PORTLAND, Ore. — Dr. Claire Wheeler joined Cristin Severance to answer your questions about the coronavirus.
Dr. Wheeler teaches Portland State University’s communicable disease course, has a specialty in Emergency Medicine and a Ph.D. in Behavioral Health.
A partial transcript of the discussion between Cristin Severance and Dr. Claire Wheeler is below.
Severance:
So, masks. I was flying yesterday. I did see some people with masks. I thought I'd see a lot more. Should people be wearing them?
Wheeler:
The only people who should be wearing masks in the community outside of healthcare settings are people with symptoms. Masks do not help asymptomatic people. In fact, masks can make the situation worse, partly because the virus can enter your body through your mouth, your nose or your eyes. And they also like the sort of moist, warm environments that a mask creates. And another fact that has been observed is that when a person's wearing a mask, they actually touch their face more often than when they don't. You're messing with it, you're adjusting, it itches, making sure it fits and it's touching your face that is probably the most risky behavior right now that people are, it's really hard not to do that. It's estimated that we touch our face about 15 to 20 times a minute. And a lot of times it's part of our emotional expression. I'm working really hard not to touch my face right now, but with the mask, it makes people touch their face more. When we wear masks in the hospital, when we're doing surgery or working in the ER, we're protecting patients from us because our droplets are blocked by that mask. But even an N-95 mask, that is if it's not professionally fitted and you know, absolutely, you know for sure that it's functioning. If you don't have the virus, it may protect you from inhaling a droplet, won't stop you from picking something up on a surface and then you go to take the mask off, what are you doing? You're touching your face. And also we're running short on mass for the people who really need them.
Severance:
Should we be avoiding crowds?
Wheeler:
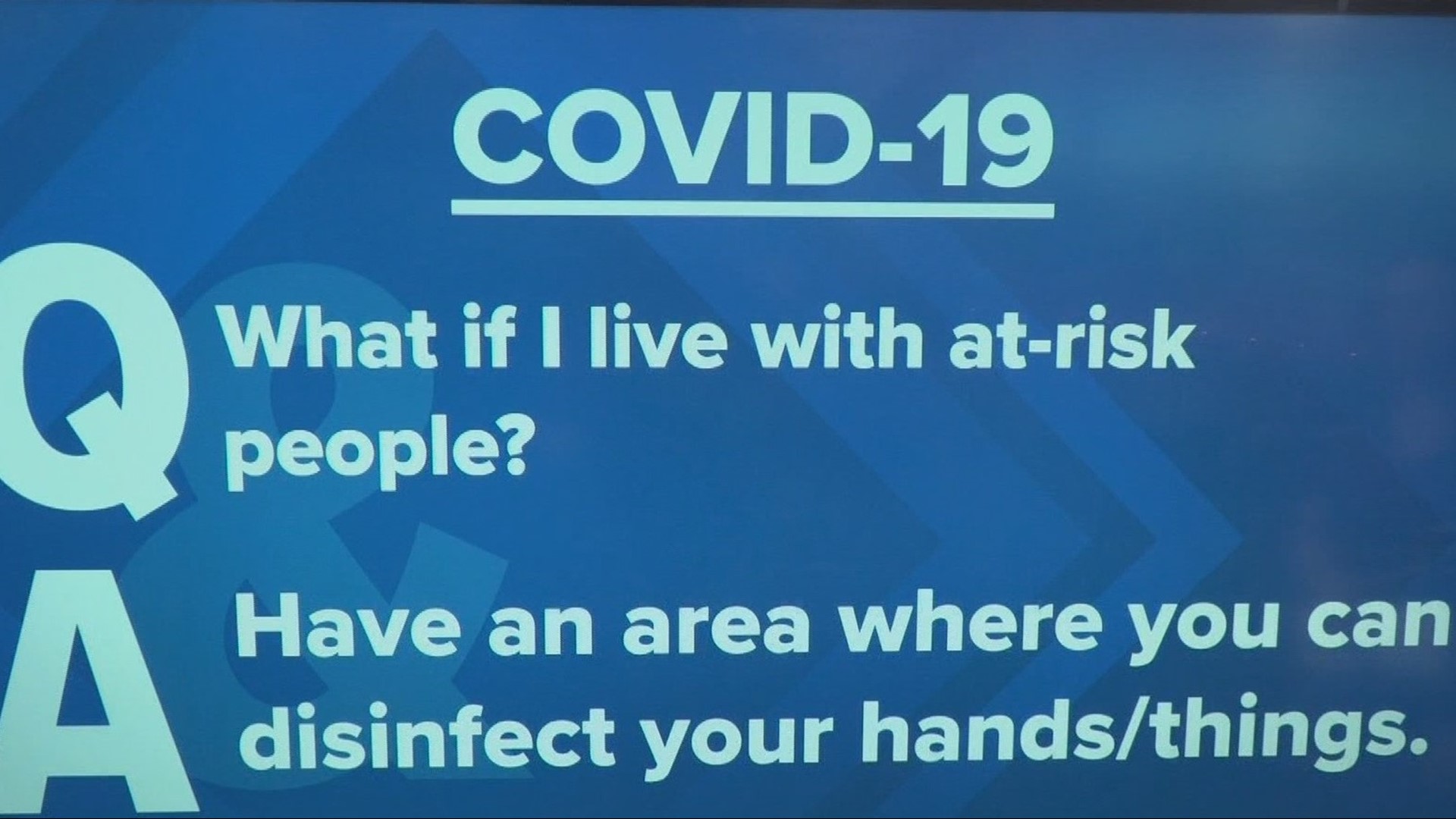
That is such a great and interesting question. And you know, as a mom and a 60-year-old woman now in that dangerous age group, I think about that and I have a visceral response to that question. Like, 'no, no, just stay home and don't go into crowded, crowded situations.' During a normal flu virus. I think, or a flu outbreak, I think it's probably wise to be at least conservative or thoughtful about where one goes in terms of crowded environments. At this point, since we don't know the extent of the spread, I think that people that particularly high-risk should consider avoiding crowds. Or if you say lived with an elderly relative that you would maybe think a little more about that person's safety. You personally might not be as much at risk, but if you bring it home to someone at risk that that's a problem.
Severance:
Is the quality of the air in an airplane cabin more conducive to getting the virus?
Wheeler:
That's also an interesting subject. I have three children and they all live away from home, and they all were going to come home for spring break and two out of three of them are not coming, which is very disappointing to me. But I support that decision. There's actually two things I think that we need to think about here: One is anxiety and the other is the reality of the situation.... What I've been reading about on airplanes is first of all, the window seat is the safest in terms of being exposed to things that are circulating in the cabin. And this has actually been tested. There's been research done on this. The aisle seat is where you're most likely to be exposed to a particle. Also, supposedly at least two rows of distance is a good buffer. So if someone is, does seem to be sick on a plane and you're on the plane, if there are more than two rows away from you, you probably won't be exposed to what is going on. But you might want to politely ask the flight attendant if there's a policy in place and what's being done for that person who's symptomatic.