KGW investigation reveals how doctors are allowed to keep practicing despite being accused of serious violations
The 'Sick Medicine' documentary examines what happens when state medical boards fail to stop doctors accused of significant wrongdoing from practicing medicine.

Patients trust their doctors with their bodies and with their health. But what happens when doctors abuse that trust?
Sick Medicine, a new investigative documentary from KGW News, examines what happens when the people charged with protecting patients and holding doctors accountable fail to do so. The documentary uncovers cases where doctors were allowed to continue practicing medicine even after being credibly accused of serious misconduct, including sexual abuse or gross negligence leading to the death of a patient.
In some cases, doctors escape their troubled pasts by simply moving states and continuing to practice medicine. KGW analyzed Oregon Medical Board records and found that of the 144 medical professionals disciplined in the state between 2012 and 2022, 28 of them went on to practice medicine in another state.
WATCH: Sick Medicine documentary
Pauletta's story
One of those doctors is Dr. Bhanoo Sharma. Our investigation found that Sharma was twice reprimanded by medical boards for negligence leading to the death of a patient. But neither board stripped Sharma of his medical license and he is still actively practicing.
In 2012, Dr. Sharma operated on a Portland woman named Pauletta Cameron.
We traveled to San Francisco to meet Pauletta’s daughter, Sonya Rivera. Sonya had been estranged from her mother for much of her adult life, but the two had just started repairing their relationship when Pauletta decided to get cosmetic surgery from Dr. Sharma.
“I didn’t know my mom was having surgery,” said Sonya.
Pauletta opted for a liposuction procedure ahead of a family reunion. If Sonya had known about her mother’s plans, she would have tried to talk her out of it because of her medical history.

Pauletta had a history of hypertension, cerebral aneurysms and potential congestive heart failure. Despite that, in May of 2012, Dr. Sharma approved her for liposuction at a Sono Bello clinic in Portland. He didn’t order any preoperative diagnostic testing, like an EKG, according to medical board records.
“She would not be considered a good candidate for a cosmetic procedure done electively in an office that's not accredited without an anesthesia provider monitoring,” said Dr. Juliana Hansen, professor and chief of plastic reconstructive surgery at Oregon Health and Science University.
KGW asked Dr. Hansen to review Pauletta’s medical file. She has no connection to Pauletta’s case or Dr. Sharma.
“She did not have normal signs even before surgery was started. Her oxygenation levels were documented to have an oxygen saturation of 80 percent. That is extremely low,” Dr. Hansen said.


Pauletta’s blood pressure and oxygen saturation dropped even lower during the 66 minute procedure, according to court records, but Dr. Sharma continued with the operation.
Following the surgery, Pauletta was still hypotensive and her oxygen level was critically depressed. Her levels were too low to be safely discharged. A nurse notified Dr. Sharma twice about the concerning vitals, according to court records, but he signed off on her release.
After 18 minutes in post-operative recovery, Pauletta was sent home under the care of her husband, Scott Cameron. Court records revealed that no one had told him about his wife’s dangerous condition. Hours later, Pauletta collapsed at home and was later admitted to the ICU.
Sonya flew to Portland as soon as she heard the news. She recalled seeing her mother hooked up to a ventilator.
“When I turned and looked at her, I was like, ‘Oh my god.’ And that’s when my knees kind of buckled and stumbled and the nurses caught me,” Sonya said.
Pauletta was in a coma for three days before Sonya had to make the difficult choice to remove her mother from life support.
“It was like my whole world was gone,” Sonya said.


Lawsuit triggers investigation
According to medical records, Pauletta had experienced cardiac arrest and congestive heart failure, along with acute respiratory failure and an anoxic brain injury. In other words, no oxygen was getting to her brain.
An autopsy reported that a traumatic bowel injury was her cause of death. Pauletta’s family filed a $13 million lawsuit and accused Dr. Sharma of perforating her bowel during the surgery.
“We do have information from her autopsy report that the deeper layers beneath the fat were punctured,” Dr. Hansen said.
The lawsuit triggered the Oregon Medical Board to investigate Dr. Sharma. Investigators found that he “engaged in conduct that constituted unprofessional or dishonorable conduct” and “gross or repeated acts of negligence.” A medical board report stated that he “unnecessarily placed” Pauletta’s “safety in jeopardy by conducting this elective procedure” and “failed to properly assess [Pauletta’s] post-op condition.”
Dr. Sharma refused to answer our questions. He initially agreed to a phone call to discuss our findings, but quickly said he would not answer questions and ended the phone call.
He did, however, defend himself in a letter to health officials. In the letter, Dr. Sharma stated he performed a complete physical exam before the surgery and believed Pauletta was a suitable candidate for the procedure. He also argued that he followed his clinic’s proper procedures for discharging a patient and that Pauletta was alert and talking when she left.

“One needs to recognize a patient who’s in distress, and when your oxygen levels are low after surgery, that patient should never be discharged to their home,” Dr. Hansen said. “She needed basic medical care that should have been recognized by any surgeon.”
When asked whether Hansen believed Pauletta’s death could have been prevented with that medical care, Hansen responded, “Absolutely.”
A second patient dies
As medical board investigators looked into Pauletta’s case, they discovered five additional patients in Oregon who needed emergency medical care after cosmetic procedures with Dr. Sharma.
The Oregon Medical Board revoked Dr. Sharma’s license in 2015, nearly three years after Pauletta died. But the medical board later reversed course for reasons it won’t disclose. Instead, the board placed conditions on his license, like imposing a fine and requiring him to complete continuing education.
Dr. Sharma eventually stopped practicing in Oregon and began operating in Illinois, where he also held a medical license.
Then, in 2016, another one of Dr. Sharma’s patients died. A 41-year-old woman died during a lipoplasty procedure in Hazelcrest, Illinois. According to medical board records in Illinois, investigators determined Dr. Sharma’s “deficient injection technique punctured muscle and gluteal veins and permitted fat to enter the bloodstream and become trapped in the lungs.”
Investigators discovered three additional patients in Illinois who had received emergency medical care after their procedures with Dr. Sharma. An investigator for the Illinois Medical Board declared him an “immediate danger to the health and safety of the public.” Still, the board chose not to revoke Dr. Sharma’s license.
Instead, the Illinois Medical Board suspended Dr. Sharma’s license for 18 months. He surrendered his license in Oregon around the same time. By this point, it had been roughly five years since the Illinois patient had died.
Despite being found to be grossly negligent in multiple cases across two states, Dr. Sharma still holds an active medical license in one state: Indiana. KGW found that he’s actively practicing there, 13 years after Pauletta’s death.
“I can’t fathom that he’s still practicing,” Sonya said.
Through a public records request, KGW learned that the Indiana Medical Board opened an investigation in 2021 after three new complaints against Dr. Sharma. However, there was no evidence of an investigation on the board’s website until spring 2023. The case is pending.
“Why is he slipping through the cracks? Why isn’t somebody doing something?” Sonya said. “Why is the medical board not seeing that this is happening? Why isn’t anybody going after him for what he’s done?”
The case of Dr. Christopher Baldwin
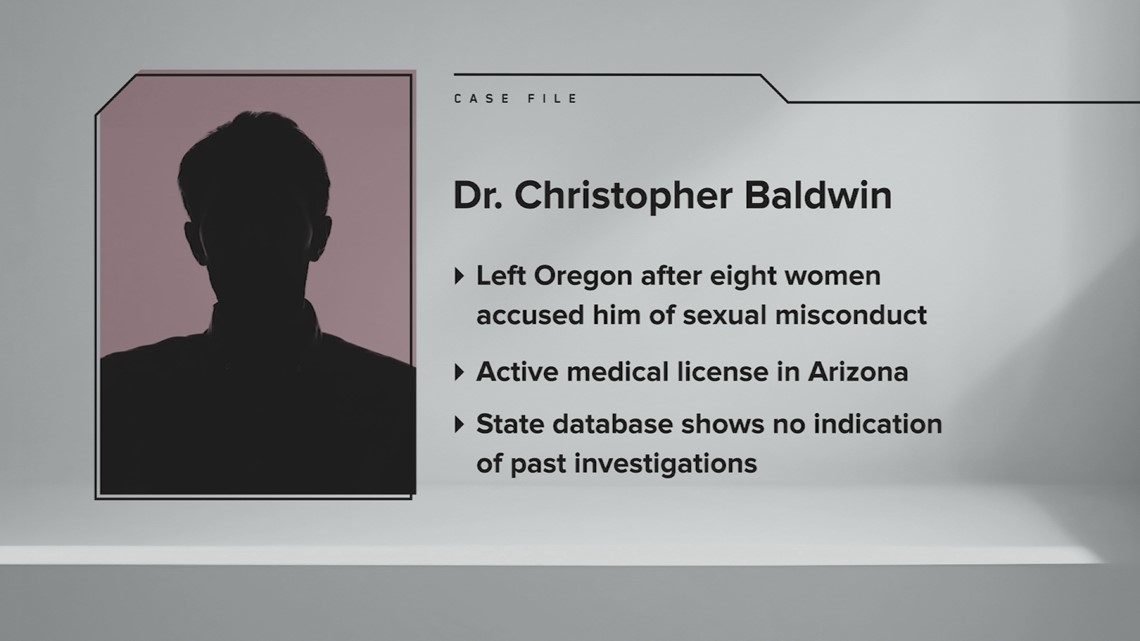
Dr. Sharma’s isn’t the only case we found where a doctor moved to a new state following a medical board investigation. Dr. Christopher Baldwin, an internal medicine physician, left Oregon after being accused of sexual battery. He now holds an active medical license in Arizona.
In 2020, eight women sued Dr. Baldwin for sexual battery and medical negligence, court records show. Six of the women were school bus drivers in Beaverton, Ore. who were required by their employer to undergo physical exams to maintain their commercial drivers’ license. In their lawsuit, the women alleged that between 2015 and 2020, Dr. Baldwin peered down their shirts during exams and stared at their breasts without legitimate medical reason. Three of the women claimed Dr. Baldwin touched their breasts or genital area.

Dr. Baldwin didn’t respond to KGW’s requests for an interview. However, he talked about the allegations during a deposition as part of the lawsuit. He denied any sexual misconduct and said, “I was not breathing heavily, but since she was wearing such a skimpy outfit, some things probably could have been semi-excited.”
It appears he settled the lawsuit confidentially and his medical license in Oregon went on “inactive” status. KGW discovered that he left the state and received a medical license in Arizona in 2022. Neither Arizona or Oregon’s medical board websites reflect evidence of the lawsuit or disciplinary action.
In the course of our reporting, KGW learned that the Oregon Medical Board issued Dr. Baldwin a “letter of concern.” The Oregon Medical Board doesn’t make such letters public, but we attempted to obtain it through a public records request.
The Oregon Medical Board denied that request, arguing the letter is confidential. We appealed that decision to the Oregon Attorney General, who sided with KGW and ordered the medical board to turn over the letter.
Instead, the medical board hired an outside law firm to fight that order in court. They are asking a judge to block the attorney general’s order and allow the medical board to keep Baldwin’s letter of concern private. The case is still pending.
Patients kept in the dark
Medical boards don’t often reveal much of past disciplinary action against doctors. It was hard enough for our team of veteran journalists to uncover the scope of the problem in Oregon, let alone across the country.
KGW filed dozens of records requests and spent thousands of dollars in records fees to get copies of what limited documents are publicly available.
We created a spreadsheet of doctors disciplined in Oregon and cross-referenced those names with disciplinary records in other states to determine which doctors continued practicing elsewhere after getting in trouble in Oregon. At best, our research gave us a limited snapshot into a nationwide problem.
KGW requested an interview with the Oregon Medical Board. We wanted to give the board the opportunity to respond to our reporting on Dr. Sharma’s and Dr. Baldwin’s cases. KGW also contacted each board member individually to weigh in on topics such as improving transparency in the way the public can request and receive information about their doctors.
The Oregon Medical Board declined an interview, citing the pending litigation it initiated with KGW. The medical board released the following statement:
“The Oregon Medical is proud of its record of upholding the agency's mission and protecting patients through consistent and decisive disciplinary actions when warranted. The Board recognizes the significant responsibility it has in investigating allegations against licensees and does so according to state law and fundamental due process rights for licensees. The Board has a zero-tolerance culture for sexual misconduct, which is demonstrated in our quarterly Board Action Reports and has been well-documented by other media outlets.”
Advocating for change
For years, patient safety advocates have been fighting for changes they believe will improve transparency and accountability both in Oregon and around the country. They want medical boards to publish all publicly available disciplinary documents online for free. There have also been calls to include more members of the public to state medical boards, which are mostly made up of physicians.
We spoke to Lisa McGiffert with the Patient Safety Action Network about changes she would like to see with the National Practitioner Data Bank. It’s the only federal database that contains information about doctor malpractice, but it isn’t open to the public. We also spoke with Oregon Sen. Ron Wyden, who helped create the database nearly 40 years ago. For more information, click here to read our full story.

Resources for patients
While there is currently no way for patients in Oregon to get a comprehensive look at their doctor’s record, you can look them up on the state’s medical board website. The Oregon Medical Board allows people to verify a current or past license, and view some disciplinary and malpractice information.
KGW also has a guide on when to report your doctor to the medical board, along with details about what the complaint and investigative processes look like.
Another helpful resource for patients is DocInfo, a free and national database of information about physicians. Patients can view details including disciplinary actions and license history.