PORTLAND, Ore. — Americans can now start ordering free at-home COVID tests from the federal government after the White House announced last week an effort to give away 500 million rapid tests to address nationwide shortages.
The federal government officially launched the COVID tests program on Wednesday, Jan. 19, but people were able to place orders online one day earlier. White House Press Secretary Jen Psaki confirmed on Tuesday that a "beta testing phase" of the ordering site had gone live as a way to test the system before the official rollout.
The Biden administration also announced last week that starting Jan. 15, private health insurers are required to cover up to eight home COVID-19 tests per month for people on their plans.
Several questions remain as some details appear to still be in the works. Here's what we have found out about and what's still unclear.
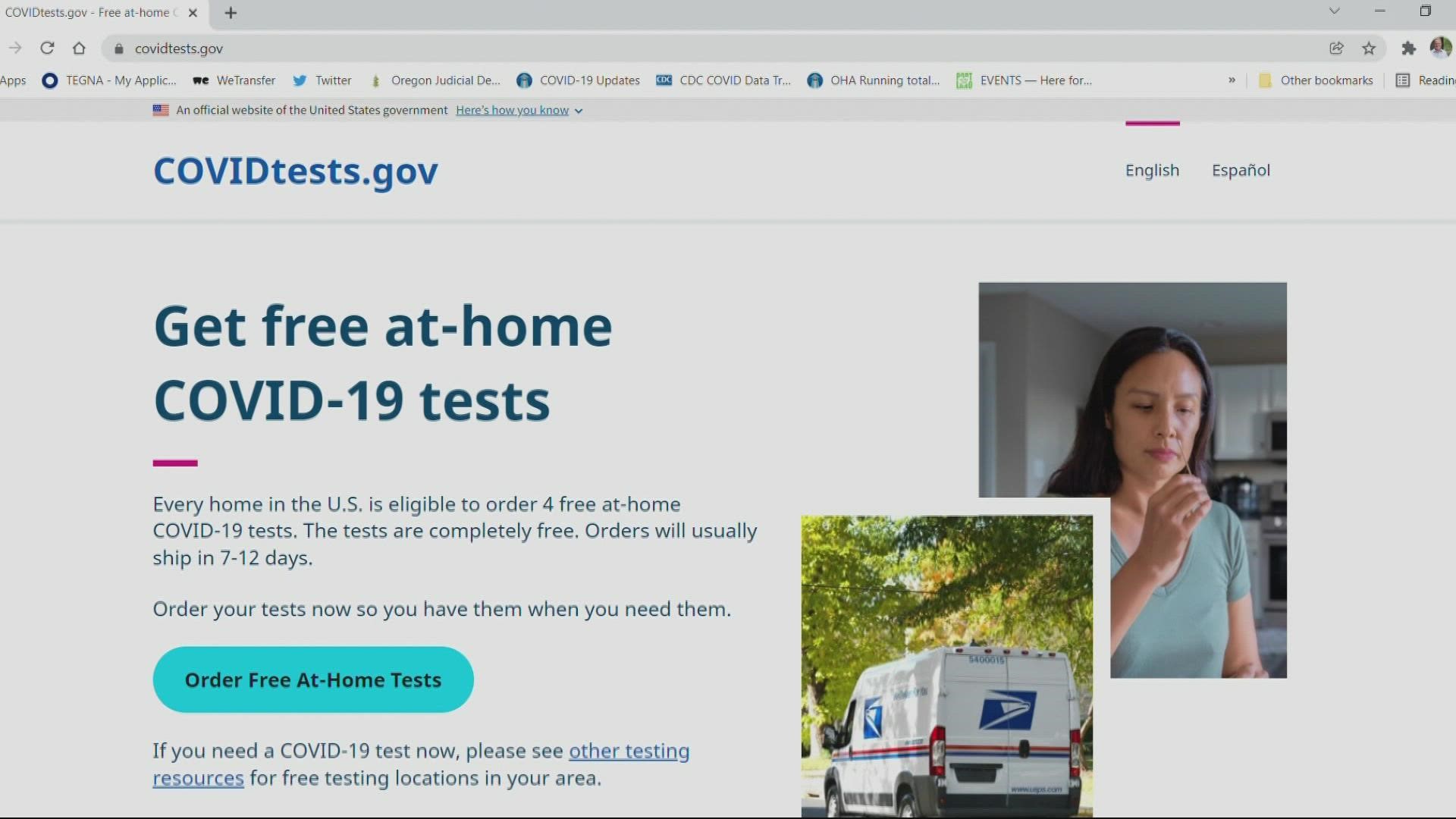
WHERE CAN I ORDER FREE AT-HOME COVID TESTS?
The website COVIDTests.gov will provide tests at no cost, including no shipping fee. You can get four tests per home.
The government also said it will offer a toll free number where people will be able to order. It's one of the ways it's hoping to ensure equity in the process, especially to communities most vulnerable.
WHEN WILL THE TESTS ORDERED ARRIVE?
The White House said “tests will typically ship within 7-12 days of ordering" through the U.S. Postal Service, which reports shipping times of 1-3 days for its first-class package service in the continental United States.
I FOUND AN AT-HOME TEST MYSELF AT A STORE OR PHARMACY. CAN I BE REIMBURSED?
Under the new policy announced last week, Americans will be able to order testing kits for free under their insurance or submit receipts for the tests for reimbursement, up to the monthly per-person limit.
Insurance has to pay for up to eight at-home tests per person per month. A family of four, for example, can be reimbursed for up to 32 tests per month.
Only tests purchased on or after Jan. 15 will be required to be reimbursed, the Biden administration said. Some insurers may choose to cover the costs of at-home tests purchased earlier, but they won't have to.
Americans on Medicare won't be able to get tests reimbursed through the federal insurance plan, but Medicaid and Children’s Health Insurance Program plans are required to cover the cost of at-home tests fully. Those who are not on a covered insurance plan can receive free tests through the forthcoming federal website or from some local community centers and pharmacies.
HOW CAN I FILE FOR REIMBURSEMENT?
First of all, make sure to save your receipts. Second, go online to see if your health insurance company has forms to reimburse you. Fair warning, not all do yet.
Regence BlueCross BlueShield of Oregon, one of the largest health insurance companies in the state, said on its website that it will reimburse up for $12 per test or $24 for a box of two tests. The website has a reimbursement form (members will need to sign into their regence.com account first). People can also download paper forms to submit via mail in Oregon and Washington. For more information, click here.
On its website, Moda Health said it will reimburse up to $12 per test bought on Jan. 15 or later. It has a reimbursement form you can fill out with your claim.
The Associated Press contributed to this report.